1801006088- LONG CASE
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I
have been given this case to solve in an attempt to understand the
topic of " patient clinical data analysis" to develop my competency in
reading and comprehending clinical data including history, clinical
findings, investigations and come up with diagnosis and treatment plan.
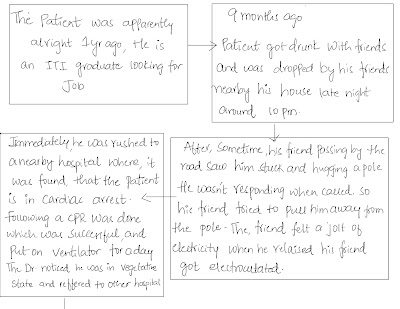
27 yr old male patient came to our hospital to seek medical advise for removal of tracheostomy tube.
HISTORY OF PRESENTING ILLNESS : -
PSYCHOLOGICAL HISTORY:-
When young, patient was a good kid and enthusiastic.
When he was 6 yrs old he lost his father (who was a heavy drinker and was a daily wage labourer ).
After this event his mother become the sole bread winner of the family.
His
brother left the house for further education, during this time the
patient started to make friends then he got addicted to alcohol.
He wasn't great with studies and used to roam jobless, he started coming to home later night.
He on his mother's request completed graduation and then started to look for a job, to support the family.
PAST HISTORY: -
● He had several episodes of seizures 3 months later following the electric shock.
● Not a known case of HTN, DM , Asthma , TB
● Tracheostomy was done.
FAMILY HISTORY:-
● Father passed away and he was a heavy drinker
● Mother :- Not a known case of HTN, DM.
Mild knee pain in both lower limbs
. while climbing stairs
● Elder Brother :- Healthy
● Sister :- Healthy
PERSONAL HISTORY:-
Height :- 5'6 --> 164.67 cms
Weight :- 40 kg approx.
Appetite :- decreased
Diet :- feeding done through Ryle's Tube
Breakfast :- Protein powder shake
Afternoon:- Rice and dal with water
Snacks:- Biscuits and milk
Dinner :- Rice and dal with water
Sleep - Adequate
Bowel and Bladder movements- regular
ADDICTIONS : -
After his brother left for his further studies, patient got new friends and new habits with it at a young age.
● Alcohol - he started when he was around 16-17 yrs old.
Quantity unknown.
● Smoking - occasionally with friends.
● Tobacco chewing - Regular. Quantity is unknown.
TREATMENT HISTORY:-
Suction every 2 hourly.
Change in position every 2 hours.
Vitals monitoring every 4 hrs.
Tab RANITIDINE 150 mg PO/OD (morning before food)
T. LEVITARECITAM 500mg PO/OD (Night time)
T. CALCITRIOL And Vit K PO/OD (after lunch)
GENERAL PHYSICAL EXAMINATION :-
Patient is in a vegetative state, uncooperative, appears thin, weak and malnourished
Pallor-Absent
Icterus- Absent
Cyanosis-Absent
Clubbing-Absent
Lymphadenopathy-Absent
Pedal edema- Absent
Koilonychia- Absent
VITALS:-
Temperature- 2 pm -> 98.4°F
4 pm -> 98.6°F
6 pm -> 98.2°F
Pulse rate- 2 pm -> 102 bpm
4 pm -> 102 bpm
6 pm -> 100 bpm
Respiratory rate- 2 pm -> 26 cpm
4 pm -> 26 cpm
6 pm -> 18 cpm
BP - 2 pm, 4 pm, 6 pm -> 110/80 mm Hg
SpO² - 2 pm , 4 pm -> 98%
6 pm -> 100%
SYSTEMIC EXAMINATION:-
CENTRAL NERVOUS SYSTEM-
● GLASGOW COMA SCALE:- E4 V2 M4 At the time of examination
● Higher mental functions -
vegetative state, disoriented
Speech, memory and intellect couldn't be assessed.
Release Reflexes :-
Grasp reflex :- couldn't be performed as patient
kept his fists clenched.
Glabellar reflex :- absent
Pout Reflex :- absent
Palmo-mental reflex :- couldn't be performed as
patient
kept his fist clenched.
● Cranial Nerve examination:-
pupillary reflex :Direct and indirect light reflex seen
Trigeminal:
Corneal and conjunctival present
Gag reflex is present
Tongue moments present
● Motor System :-
Right Left
UL LL UL LL
Bulk wasted wasted wasted wasted
Tone hypertonia normal hypertonia normal
Power :- Not able to elicit not able to elicit
Reflexes :-
Biceps, Triceps, Supinator reflexes are absent
Knee reflex positive in both limbs
Ankle reflex positive in both limbs
Plantar reflex positive in both limbs
● Sensory System :- couldn't be elicited
● Myoclonic jerks are seen regularly
● Gait:- couldn't be elicited
CARDIOVASCULAR SYSTEM :-
S1 and S2 are heard.
No murmurs are heard
Apex beat felt at 5th ICS
RESPIRATORY SYSTEM :-
B/L basal crepitations are heard
ABDOMINAL SYSTEM:-
Soft and non tender
ENT EXAMINATION:-
Nose :-
External frame work is normal.
DNS to left is noticed.
Ryle's tube in the right nasal cavity.
Oral cavity and Oropharynx:
Couldnot be examined as patient is not co-operative.
Trachea:-
Central
Tracheostomy tube was placed
INVESTIGATIONS:-
X- RAY of neck :-
Chest X Ray :-
MRI:-
PROVISIONAL DIAGNOSIS :-
Hypoxic Ischemic Brain Injury Post CPR state
TREATMENT PLAN:-
After Neurology consultation , The Neurologist suggested for Family Counselling and Palliative Therapy.




.jpeg)
.jpeg)
-2.jpg)
Comments
Post a Comment